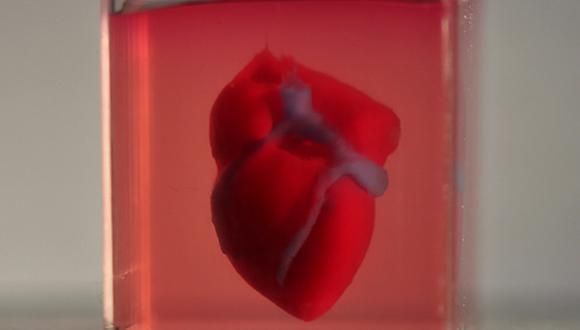
TAU scientists print first ever 3D heart using patient’s own cells
In a major breakthrough, engineered heart completely matches the cellular and anatomical properties of the patient
In a major medical breakthrough, Tel Aviv University researchers have "printed" the world's first 3D vascularised engineered heart using a patient's own cells and biological materials. Until now, scientists in regenerative medicine — a field positioned at the crossroads of biology and technology — have been successful in printing only simple tissues without blood vessels.
"This is the first time anyone anywhere has successfully engineered and printed an entire heart replete with cells, blood vessels, ventricles and chambers," says Prof. Tal Dvir of TAU's School of Molecular Cell Biology and Biotechnology, Department of Materials Science and Engineering, Center for Nanoscience and Nanotechnology and Sagol Center for Regenerative Biotechnology, who led the research for the study.
Heart disease is the leading cause of death among both men and women in the United States. Heart transplantation is currently the only treatment available to patients with end-stage heart failure. Given the dire shortage of heart donors, the need to develop new approaches to regenerate the diseased heart is urgent.
"This heart is made from human cells and patient-specific biological materials. In our process these materials serve as the bioinks, substances made of sugars and proteins that can be used for 3D printing of complex tissue models," Prof. Dvir says. "People have managed to 3D-print the structure of a heart in the past, but not with cells or with blood vessels. Our results demonstrate the potential of our approach for engineering personalized tissue and organ replacement in the future."
Research for the study was conducted jointly by Prof. Dvir, Dr. Assaf Shapira of TAU's Faculty of Life Sciences and Nadav Moor, a doctoral student in Prof. Dvir's lab.
"At this stage, our 3D heart is small, the size of a rabbit's heart," explains Prof. Dvir. "But larger human hearts require the same technology."
The secret to a new heart
For the research, a biopsy of fatty tissue was taken from patients. The cellular and a-cellular materials of the tissue were then separated. While the cells were reprogrammed to become pluripotent stem cells, the extracellular matrix (ECM), a three-dimensional network of extracellular macromolecules such as collagen and glycoproteins, were processed into a personalized hydrogel that served as the printing "ink."
After being mixed with the hydrogel, the cells were efficiently differentiated to cardiac or endothelial cells to create patient-specific, immune-compatible cardiac patches with blood vessels and, subsequently, an entire heart.
According to Prof. Dvir, the use of "native" patient-specific materials is crucial to successfully engineering tissues and organs.
"The biocompatibility of engineered materials is crucial to eliminating the risk of implant rejection, which jeopardizes the success of such treatments," Prof. Dvir says. "Ideally, the biomaterial should possess the same biochemical, mechanical and topographical properties of the patient's own tissues. Here, we can report a simple approach to 3D-printed thick, vascularized and perfusable cardiac tissues that completely match the immunological, cellular, biochemical and anatomical properties of the patient."
What organ would you like?
The researchers are now planning on culturing the printed hearts in the lab and "teaching them to behave" like hearts, Prof. Dvir says. They then plan to transplant the 3D-printed heart in animal models.
"We need to develop the printed heart further," he concludes. "The cells need to form a pumping ability; they can currently contract, but we need them to work together. Our hope is that we will succeed and prove our method's efficacy and usefulness.
"Maybe, in ten years, there will be organ printers in the finest hospitals around the world, and these procedures will be conducted routinely."